Privatisation of Healthcare
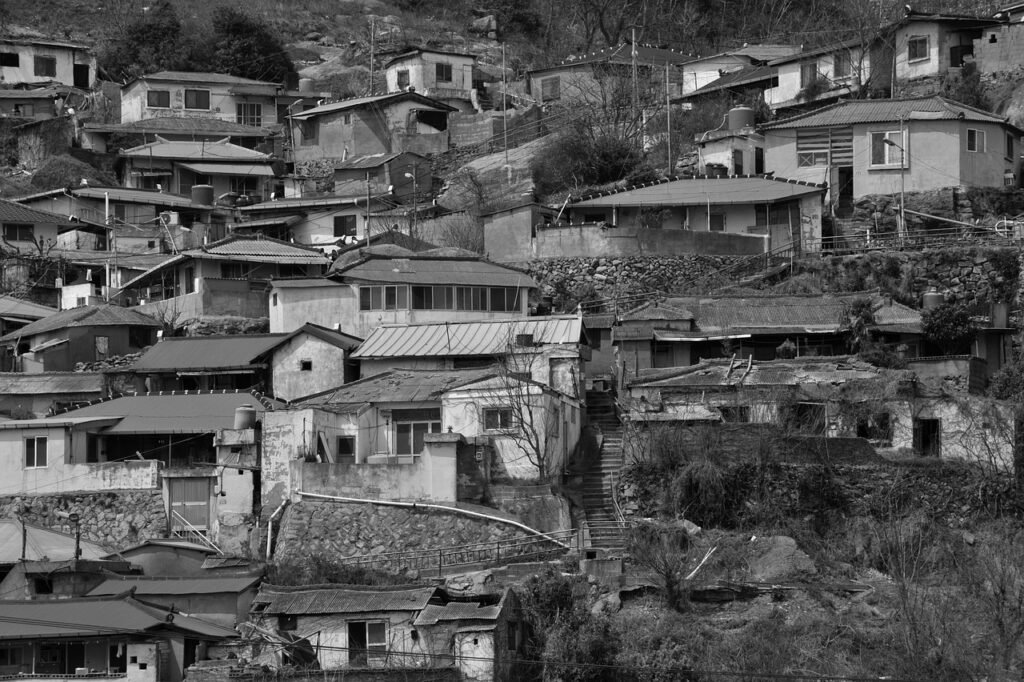
Introduction The debate surrounding the privatisation of public healthcare has intensified in recent years. Governments and academics alike are assessing the pros and cons of private versus public healthcare systems. The rise of the for-profit sector has introduced market-driven principles, such as variable insurance pricing, which have disrupted the public sphere. The increasing influence of privatisation and liberalisation has also limited the state’s ability to formulate independent policies across various sectors, including healthcare. Right to Health The World Health Organization (WHO) defines the right to health as encompassing physical, mental, and social well-being. According to WHO, health is not merely the absence of disease but a positive state of well-being that includes a joyful attitude and acceptance of life’s responsibilities. In India, while the Constitution does not explicitly guarantee health as a fundamental right, it mandates the state to provide healthcare to its citizens. Articles 39, 41, and 47 of the Constitution impose an obligation on the state to create sustainable models ensuring public health. The National Health Policy (NHP) of 2017 aligns with global healthcare trends, aiming to shift the focus from “sick care” to “wellness” by emphasizing prevention and health promotion through a strengthened public health system. Public-Private Partnership (PPP) Model in Healthcare Despite improvements in India’s public health system, significant challenges persist, primarily due to: To address these challenges, the government, in collaboration with NITI Aayog and the World Bank, has proposed a PPP model. This approach is positioned not as privatisation but as a strategic procurement of secondary and tertiary healthcare services, focusing particularly on non-communicable diseases (NCDs). The Cuban Model: A Preventive Approach Cuba’s healthcare model prioritises prevention over treatment, adopting a social rather than technological perspective. The government assigns doctors or medical teams to specific regions, making them responsible for monitoring and addressing public health concerns. They proactively track high-risk cases, such as diabetes and pregnancies, referring patients to specialized health centers when necessary. While India has a similar model, its implementation remains reactive rather than proactive. The disparity is particularly evident in rural areas, where health centers and medical expertise are scarce. Furthermore, corruption and absenteeism among rural healthcare providers exacerbate the crisis. The Cuban model’s success is attributed to strong political will, substantial government investment, and a commitment to universal healthcare. Concerns Over Privatisation Historical data suggests that market-driven healthcare models often compromise equity. In the United States, for example, healthcare privatisation led to a 30% rise in uninsured individuals in the 1980s and a 15.6% increase in the 1990s. By 1998, approximately 44 million Americans, including ethnic minorities, the poor, and the elderly, were uninsured. The inability to afford insurance directly impacts access to preventive care and chronic disease management. Privatisation in India has similarly created a divide between urban and rural populations. While private healthcare facilities thrive in urban centers, rural areas remain neglected due to lower demand and affordability issues. Private hospitals often deny services to those unable to pay upfront fees, underscoring the need for government intervention. A regulatory framework is essential to ensure affordability, either through subsidies or state-sponsored insurance for economically disadvantaged citizens. Policy Recommendations To ensure equitable healthcare access, the government must: Conclusion Healthcare is a fundamental necessity, not a privilege. While privatisation may improve efficiency, it often overlooks the affordability aspect for lower-income populations. Instead of relying on private models to handle costliest treatments like cardiac and cancer care, the government must assume greater responsibility. A well-structured, publicly funded healthcare system, complemented by a regulated private sector, is essential for ensuring universal access to quality healthcare in India.
Privatisation of Healthcare Read More »